- Genetic samples remotely collected as part of uMed’s AccessPD Cohort to contribute to the international GP2 Program.
- Analyses of samples will be linked back to the AccessPD Core clinical dataset (combining electronic health record data and patient reported outcomes), providing PD researchers with comprehensive resources.
- AccessPD supports GP2’s mission to expand sample collection from groups traditionally under-represented in PD genetics studies.
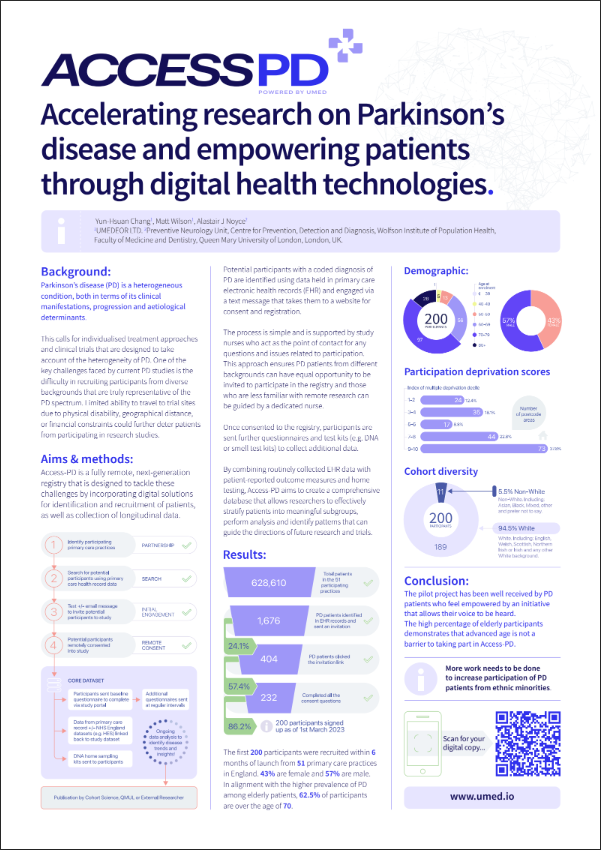
Cambridge, MA, June 18 – Healthcare evidence-generation and technology company uMed today announced they have entered into a partnership with the Global Parkinson’s Genetics Program (GP2) to support expansion of the international genetic initiative. uMed will be providing access to genetic samples collected as part of their AccessPD Cohort Study.
The Aligning Science Across Parkinson’s (ASAP) initiative launched GP2 in 2019, building on previous funding efforts from The Michael J Fox Foundation for Parkinson’s Research (MJFF). ASAP is a coordinated research initiative to advance targeted basic research for Parkinson’s disease (PD). ASAP is devoted to accelerating the pace of discovery and informing the path to a cure for PD through collaboration, research-enabling resources, and data sharing.
AccessPD is a unique Cohort Study of patients diagnosed with PD, that remotely collects data from pre-consented patients at home and links with EMR and clinical data to build a comprehensive regulatory grade dataset that can be further augmented with custom endpoints.
Under the announced agreement, uMed will be contributing anonymized genetic samples, remotely collected from consented participants within AccessPD.
GP2 will perform genetic analyses of the samples to feed into the program, and results will also be linked back to additional endpoints within the AccessPD clinical dataset including ePROs, eClinROs, EHR and device data.
The ongoing collection of genetic samples is part of the AccessPD protocol. uMed observes on average a 72% completion rate of the saliva-based genetic tests sent to patients within the cohort, highlighting the formidable engagement of participants, and the strength of uMed’s ACCESS Cohort model to build patient communities and encourage participation and retention.
Dr Matt Wilson, CEO & Founder at uMed commented “We’re delighted to be contributing to the GP2 program and excited about the impact that this partnership will have on AccessPD and the future of Parkinson’s research. AccessPD already provides researchers with a comprehensive picture of the patient, and this partnership with GP2 allows us to expedite the expansion of this rich dataset. It’s programs like AccessPD and GP2 that will be game changing to research in the future, and we are proud to be part of the process!”
In alignment with GP2’s mission to expand global genetics studies to include populations underrepresented in research, AccessPD’s unique decentralized approach will maximise the involvement of these populations in the program.
AccessPD is underpinned by uMed’s ACCESS Research Platform which is embedded across an expansive network of healthcare institutions across the US and UK, and allows for engagement with patients on behalf of the healthcare provider. Combined with the remote collection of data from patients at home, this approach provides access to large patient populations, including those that would normally face economic, geographical and disease-related barriers.
Press release on prweb.com
Find out more about AccessPD here, or chat to our team to discover how AccessPD can support your research goals.